Common sources of heel pain are Haglund's Deformity, heel calluses, heel fissures, and plantar fasciitis (heel spurs).
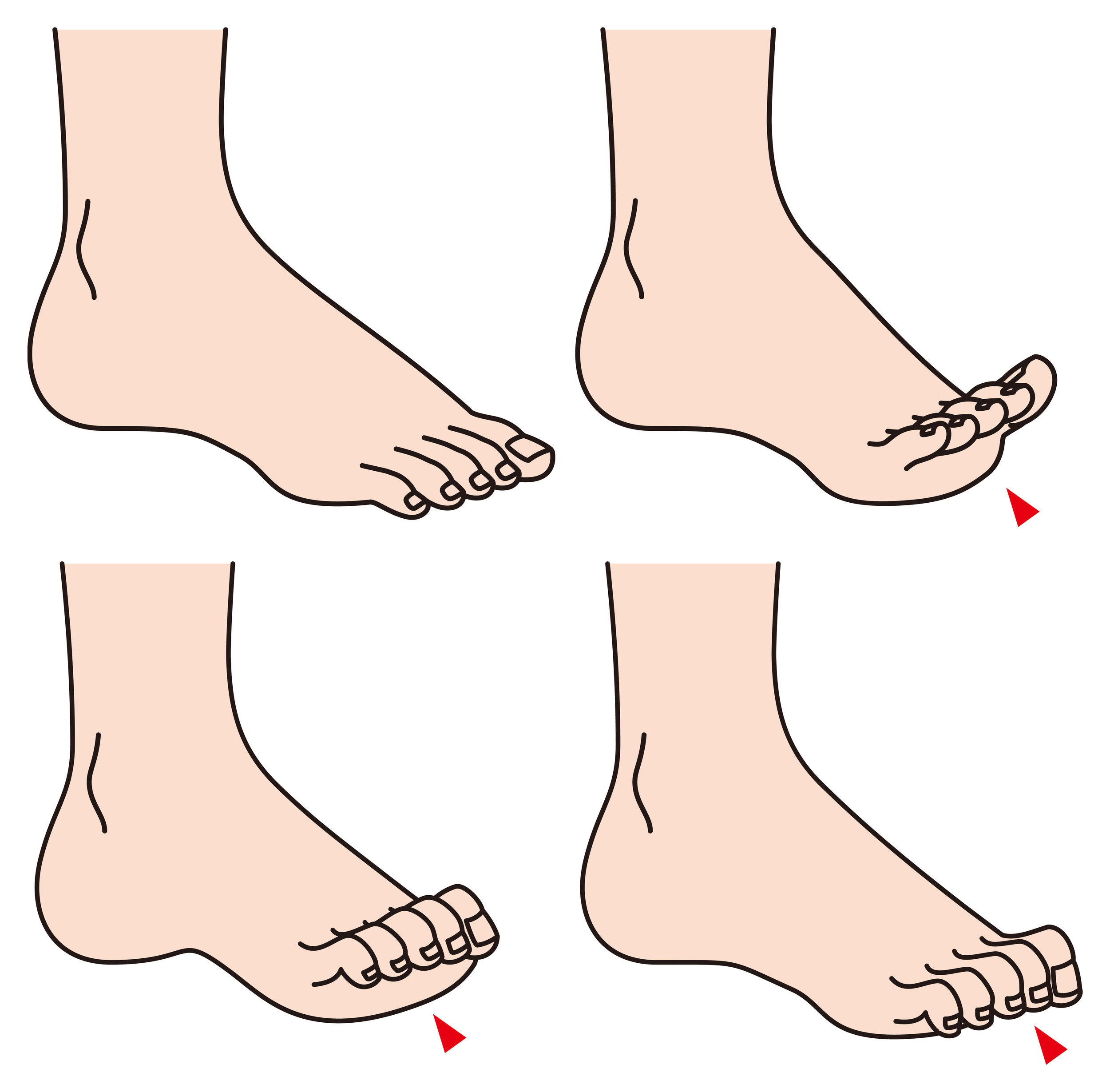
Haglund's Deformity
Haglund's Deformity (also known as pump bump or retrocalcaneal bursitis) is a painful enlargement on the back of your heel bone that gets irritated by shoes. You might see a red, painful, and swollen area at the back of the heel. It's more common in women because of wearing high heels. To address this foot problem, you can change shoes, soak your feet, or use anti-inflammatory medicine, but check with your podiatrist first.
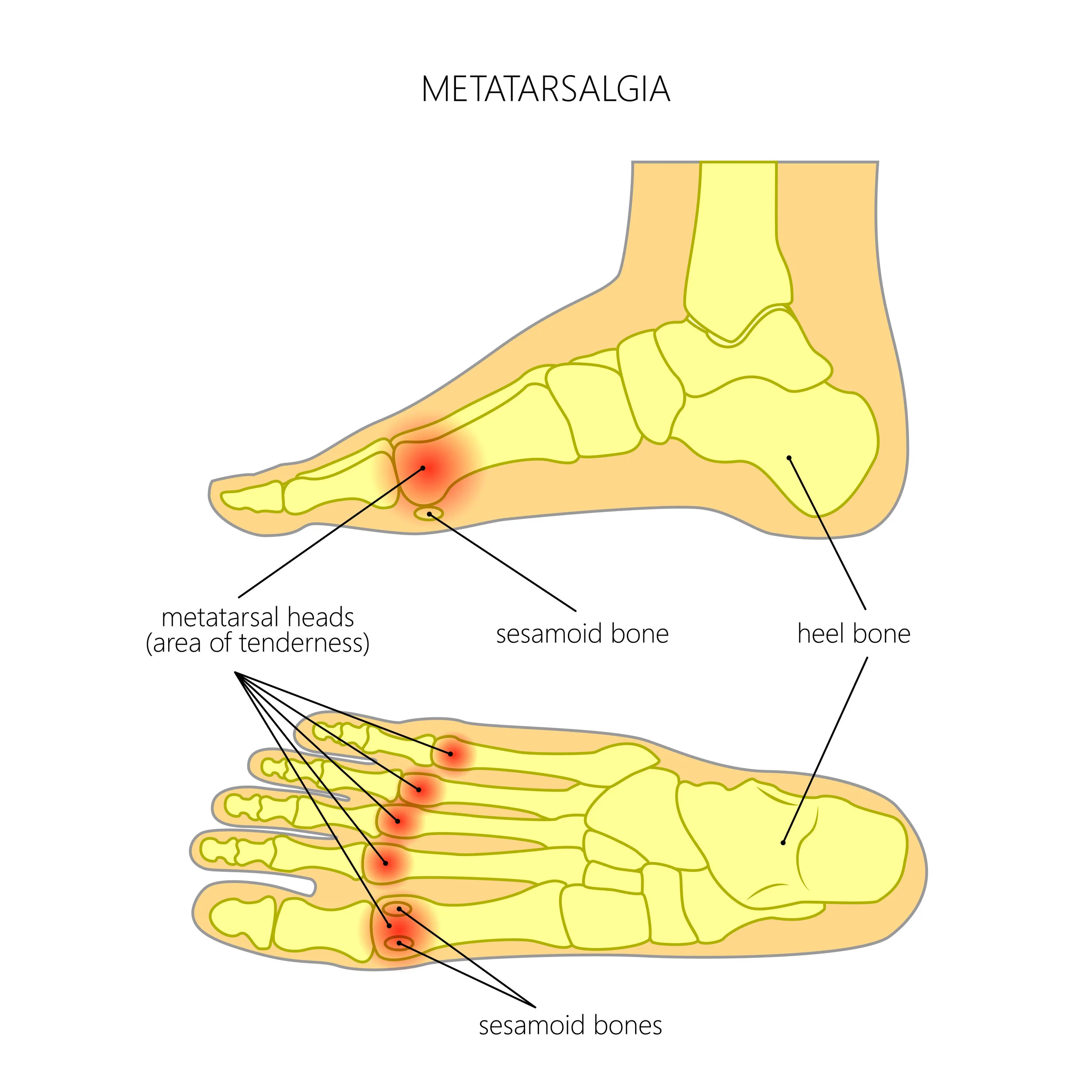
Heel calluses
Heel or plantar calluses develop when one metatarsal bone is longer or lower than the others and it hits the ground with more force. Your skin under this bone thickens and causes irritation.
Heel calluses can usually be treated without surgery. In severe cases, a surgery called an osteotomy is performed to relieve the pressure on your bone.
Heel fissures
When the skin on your heels cracks and bleeds, we call it heel fissures. This can be caused by wearing open-backed sandals or shoes that allow your heel to slip when you walk. Skin conditions like eczema and psoriasis can also lead to heel fissures. It's important to wear proper shoes to prevent heel fissures. Using deep skin moisturizers and lotions can help your foot to heal.
Plantar fasciitis
Most heel or arch pain is caused by a condition called plantar fasciitis, which means an inflammation on the bottom of your foot. Inside your foot a connective tissue called the plantar fascia stretches from the base of your toes, across the arch of the foot, into the heel bone. If your foot rolls inward excessively when you walk, this is called overpronation, and it causes plantar faciitis. This puts added tension on your plantar fascia and causes inflammation and pain.
We treat plantar faciitis heel pain with anti-inflammatory medications, ice packs, stretching exercises, orthotic devices, and physical therapy. In persistent cases, Extracorporeal Shock Wave Treatment (ESWT) may be used to treat the heel pain.